Did you know that healthcare professionals see 20 to 30 patients on average every day?
This number will only rise as the $9.46 billion global online consultations market expands. Efficient note-taking strategies are becoming a must-have rather than a good-to-have to effectively manage a high volume of patient information and deliver accurate diagnoses and treatment plans.
And that’s where the SOAP methodology makes all the difference.
Though a widely recognized note-taking approach for healthcare workers, SOAP notes demand a comprehensive understanding to ensure proper healthcare. This guide will show you how to write SOAP notes. From the basic concepts and application to overcoming challenges, we’ll cover all you need to know about the SOAP methodology.
What Is a SOAP Note?
⭐ Featured Template
Struggling to keep SOAP notes organized? ClickUp’s free Medical Chart Template makes documentation quicker, clearer, and stress-free.
A SOAP note is a problem-oriented medical record healthcare professionals use to document patient appointments and clinical sessions. Among several note-taking methods, such as the Cornell note-taking, outline method, and mapping approach, SOAP is most suited for medical consultations.
SOAP is an acronym for four headings: Subjective, Objective, Assessment, and Planning. The approach starts with what the patient is experiencing and ends with an informed action plan to ensure the highest-quality care is delivered.
Basics of Writing SOAP Notes
Overview of the SOAP process:
- Subjective: The patient’s main complaint, how it has developed, and all relevant history, such as medical records, ongoing medication, state of mind, etc.
- Objective: Vitals, diagnostic tests, lab results, etc.
- Assessment: A diagnosis and documented findings
- Planning: Next steps, such as prescription, follow-up tests, consult or referral, etc.
With a brief overview of the approach, here is a breakdown of the SOAP note format with examples to help you understand its purpose:
S: Subjective
This heading of the SOAP note records the patient’s personal views or feelings.
The fundamental purpose of the ‘Subjective’ heading is to understand the issue(s), symptoms, and their development as described by the patient. Medical professionals often include direct quotes from the patient here.
These are the three key aspects you must document here:
Part I: Chief complaint
This is the patient’s main issue and serves as the note’s primary topic. It could be a symptom, condition, or previous client’s diagnosis that elaborates on why they’ve come to you.
Remember, the patient may have more than one chief complaint.
Part II: Development of present illness
Here, you should record how the situation developed and what influences it. To keep this relevant and your notes organized, here’s what both clinicians and therapists should record:
- Onset: When did the chief complaint begin?
- Location: Where is the pain or problem located?
- Duration: How long has the patient been facing this?
- Characterization: How does the patient describe the issue?
- Alleviating and aggravating factors: What makes the condition better and worse?
- Radiation: If it is pain, does it move or stay in one location?
- Temporal factor: Is the problem worse (or better) at a particular time of the day?
- Severity: On a scale of 1 to 10, 1 being the least and 10 being the worst, how does the patient rate the chief complaint?
Part III: Record history
Here’s what must be included:
- Medical history: Record current or past medical conditions
- Family: Gather pertinent family history based on the nature of the condition
- Surgical: Document details about recent surgeries
- Social: Add relevant information on the environment, eating habits, physical activities, and mental state of mind
- Current medications and allergies: Make sure to take note of ongoing medication with dosage and allergies
Each of these sections often helps uncover symptoms not otherwise mentioned by the patient, such as weight loss, abdominal pain, emotional fluctuations, or muscular issues.
Here are three examples of chief complaints:
- Medical: Patient complains of severe headache and nausea
- Therapy: The patient reports feeling anxious and overwhelmed about an upcoming job interview
- General: The patient states they have been experiencing difficulty sleeping
Following this, you should record the history and development of the chief complaint.
O: Objective
This involves collecting measurable data from the patient through instruments, reports, and examinations.
Here are the key forms of objective data:
For clinicians
- Vital signs: Blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation
- Physical exam findings: Appearance, demeanor, and results of physical examinations, such as tenderness, sensitivity, and main areas of pain
- Lab tests: Reports from blood tests, urine analysis, and other relevant laboratory results
- Imaging results: X-rays, CT scans, MRIs, and sonography
- Other diagnostic data: Electrocardiograms (ECGs), pulmonary function tests, and psychological assessments
- Review of past files: Acknowledging and transferring records and recommendations shared by previous doctors
For therapists
- Appearance and demeanor: Eye contact, body language, and overall presentation
- Speech patterns: Any hesitations, rapid speech, or unusual vocal tone
- Thought processes: Ability to stay on topic, organize thoughts, and problem-solve
- Mood and affect: Patient’s emotional state and how they express it
- Behavior: Any unusual or significant behaviors during the session
- Mental status exam findings: Test and survey results regarding orientation, memory, attention, and other cognitive functions
The primary focus behind the objective heading is to record signs and factual evidence that helps you correlate the patient’s complaints and symptoms.
Here is an example relevant to clinicians:
- Vital signs: BP 120/80 mmHg, HR 80 bpm, RR 18 breaths/min, Temp 98.6°F, O2 Sat 98% on room air
- Physical exam: Alert and oriented x3, no acute distress, heart sounds regular, lungs clear to auscultation, abdomen soft and non tender, no edema in extremities
- Lab results: WBC 8,000/mm³, Hb 12 g/dL, Hct 36%, Plt 200,000/mm³
- Imaging: Chest X-ray unremarkable
Here’s an example for therapists:
- Client appearance: Dressed formally, made good eye contact, appeared anxious
- Speech: Clear, coherent, slightly pressured
- Mood and affect: Reported feeling depressed and irritable
- Behavior: Restless, fidgeting with hands
- Mental status: Oriented to person, place, and time
While objective findings are numerous, keep your notes focused on the chief complaint to avoid information overload.
A: Assessment
The third element is the product of both subjective and objective sections. Medical professionals must record an assessment of the patient’s status. It involves the following three steps:
- Correlating subjective notes with objective records
- Reviewing possible interactions of the issues in case there are multiple complaints
- Noting changes in the status of the problems over time
To record the assessment, this is the ideal structure:
- Diagnosis: A list of all possible diagnoses in order of likelihood
- Summary of findings: The thought process behind each diagnosis, leading to a justified action plan
Here is an example for clinicians:
- Differential diagnosis: Acute bronchitis, pneumonia, asthma exacerbation
- Summary of findings: The patient presents with a history of cough, fever, and fatigue. Physical exam reveals rhonchi in bilateral lung bases
Here is an example for therapists:
- Differential diagnosis: Major depressive disorder, adjustment disorder with depressed mood, generalized anxiety disorder
- Summary of findings: The client presents with symptoms of depressed mood, anhedonia, difficulty concentrating, and insomnia. There is no significant history of anxiety or panic attacks
P: Planning
The final section of your SOAP note addresses the plan of care. It would be best to detail the need for additional testing or a consultation with other clinicians.
Here are the key elements of planning in your SOAP note:
- Tests needed: The name of the test, conditions, and the next steps based on the test results
- Therapy or medication: Prescriptions, if any
- Specialist referral(s) or consults: A referral, in case the scope falls under another specialization
- Counseling: Suggestions for the patient on how to take better care
An example for clinicians diagnosing pneumonia:
- Tests needed: Chest X-ray to confirm pneumonia, sputum culture to identify cause, complete blood count (CBC) to assess infection severity
- Therapy or medication needed: Amoxicillin 500mg TID for five days, lots of fluids, and rest
- Specialist referral(s) or consults: If symptoms worsen or there is no improvement after three days, consider referral to pulmonology
- Counseling: Educated the patient on the importance of antibiotics, signs of improvement, and when to seek emergency care
An example for therapists:
- Test needed: There is no need for additional examinations
- Therapy or medication needed: 6 weeks of cognitive-behavioral therapy (CBT) for depression. Discuss potential benefits and side-effects of antidepressant medication
- Specialist referral(s) or consults: None as of now
- Counseling: Educated the patient about depression, symptoms, and treatment options
While the planning section is the end goal for every note, it also helps future physicians understand the treatment approach.
Specific applications of SOAP notes
With the four headings in mind, here are three specific applications of SOAP notes:
SOAP notes for mental disorders
Applying SOAP notes to document a patient’s mental health condition gives structure to a very subjective field.
Here is how to effectively focus SOAP notes on mental disorders:
- Subjective data record symptoms like mood, anxiety, or suicidal thoughts
- Objective findings might involve behavior, speech patterns, or appearance
- Assessment focuses on diagnosing the disorder
- Planning covers care through therapy, medication, and follow-up
SOAP notes for physical therapy
Physical therapy is more direct and quantified with SOAP notes. Medical professionals use them as progress notes as well.
Here’s the overview of what notes physical therapy entails:
- Subjective data includes pain levels and functional limitations
- Objective findings involve scans and measurements like range of motion and strength
- Assessment determines treatment effectiveness and sets goals
- Planning will focus on exercises, modalities, and patient education
SOAP notes for handling emotional abandonment
SOAP notes help systematically address and document healthcare in scenarios like emotional abandonment, which require long-term treatment.
Here’s how to adapt your note-taking when addressing abandonment issues:
- Subjective data record feelings of loss, betrayal, and loneliness
- Objective findings might observe and quantify levels of withdrawal or anger
- Assessment will identify the severity of emotional impact, potential coping mechanisms, and priority of developing an action plan
- Planning focuses on therapy and exercises to build trust, develop healthy coping strategies, and explore healthy relationships
Documentation Requirements for Video Telehealth
Here are five reasons why documentation through SOAP notes is so vital:
- Ensures legal and ethical compliance
- Streamlines reimbursement for insurance claims
- Builds detailed records that facilitate patient interactions for future reference
- Serves as evidence in case of legal disputes or malpractice claims
- Facilitates better diagnosis and treatment plans
With this in mind, cover these critical details in your SOAP notes, especially over an online consultation:
- Patient identification: Verify patient identity using secure methods
- Patient location: Record the patient’s location for legal and billing purposes
- Informed consent: Document the patient’s understanding of the process and consent for treatment
- Follow-up: Document any scheduled follow-up appointments or referrals
- Signature and date: Apply an electronic signature and date to the telehealth encounter note
Challenges in Writing SOAP Notes and How to Overcome Them
The SOAP methodology is a note-taking structure with a systematic approach. It is highly effective for handling sensitive information but is challenging to master without some foresight.
Here are four challenges you might face with your SOAP notes and tips to improve their impact:
1. Understanding and addressing jargon
Technical jargon creates a barrier to effective communication, client trust, understanding of diagnoses, and compliance with treatment plans.
Here are some practices that will help prevent misunderstandings:
- Use clear, simple language to foster trust through open communication
- Encourage questions and empower patients with information
- Match language to the patient’s understanding when jotting down medical terms
2. Balancing detail and clarity
Balancing between informative and clear notes can be a challenge, impacting the effectiveness of treatment and diagnosis.
To overcome this tug of war, here are two tips to remember:
- Focus only on relevant details to help efficiently connect symptoms, causes, and treatment
- Use standardized templates or guidelines to structure your notes efficiently
3. Time constraints
Limited time for patient interaction and fresh documentation often leads to rushed and incomplete notes. This challenge impacts the overall quality of understanding and treatment.
Here are practices that facilitate time management without hindering the quality of healthcare:
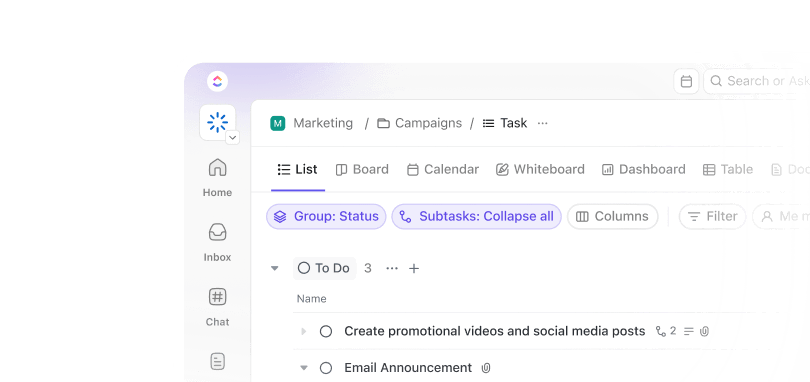
- Streamline your note-taking process with project management platforms like ClickUp
- Cultivate efficient note-taking habits, such as focusing on key points and prioritizing essential information
- Delegate certain documentation tasks to administrative staff before and after the appointment begins
4. Subjective vs. objective information
Accurately differentiating between subjective patient reports and objective findings is crucial for effective SOAP note development and treatment planning.
Here are three practices you must incorporate during note-taking to stay on track and segment information effectively:
- Use clear headings for each section of the SOAP note
- Develop regular training modules for yourself and relevant staff to accurately document subjective and objective data without prejudice or assumptions
- Utilize standardized assessment tools to measure objective findings consistently
How to Write SOAP Notes
For an effective SOAP note, adopting a project approach ensures a clear and detailed form of documentation. We’ve put together some helpful tips on writing impactful SOAP notes and also tools you can use for this.
1. Create and manage your SOAP notes
Digital note-taking apps offer the advantage of accessible patient notes. They also mitigate the risk of physical record-keeping and help medical providers manage health records better. With this in mind, the first step to creating and managing your SOAP notes is to adopt a robust tool.

ClickUp Docs is a platform documentation tool that helps you record observations and treatments. Its banners and font formatting features allow you to structure your SOAP heading for easier navigation and review. With ClickUp Docs, you can also instantly link tasks such as lab tests, referrals, and prescriptions for your administrative staff to prepare.

ClickUp Notepad is a go-to quick note tool for your consultations. Its instant accessibility allows you to take care of patients who walk in without an appointment or come through as emergencies. Like ClickUp Docs, it also lets you convert any point into a task linked with a project.
All of ClickUp’s tools come with real-time tracking, instant sharing, and even printing, so multiple doctors and emergency medical technicians involved in the case have no issues accessing and updating relevant results.
2. Visualize your SOAP notes
Many consultations include tests such as X-rays, MRIs, and blood work. Visualizing all the results within your notes is an advantage that saves time and highlights any significant developments.

ClickUp Whiteboards is like a virtual soft board where you can visualize notes and treatment plans and add reports to improve patient understanding. ClickUp Whiteboards is also helpful for doctors, nurses, and other healthcare professionals to observe how a patient’s health has developed.
This visualization is also key for presenting your meeting notes during improvement workshops and healthcare conferences.
3. Empower your SOAP notes with AI
While a personal touch is integral to experience-driven consultations, adding AI note-taking tools to your SOAP notes can help you work more efficiently.

ClickUp Brain is the ideal AI partner for your SOAP notes. It helps manage your databases to retrieve patient details efficiently. ClickUp Brain also simplifies medical jargon into terms that your patient will comprehend with its AI Writer for Work.
Another key advantage to this tool is that it instantly generates the latest updates and summaries on the patient’s progress within your ClickUp Doc or Notepad.
4. Streamline and standardize with templates
A standardized SOAP note template for your notes can take your healthcare service quality and efficiency to the next level.
The ClickUp Medical Chart Template is a framework that simplifies the consultation process. With its pre-designed structure, adding vitals, patient history, and special conditions takes just a few clicks. The template also allows you to assign and delegate tasks within the document to your staff in case you want an expedited report.
ClickUp’s Patient Management Template is another framework for managing appointments. This easy-to-use template focuses on storing patient information and scheduling appointments. Essential details such as name, age, insurance coverage, address, medications, and conditions are easy to add and monitor.
ClickUp also allows you to integrate this data into note formats, making the subjective heading of your SOAP notes less time-consuming and efficient.
Elevating Healthcare Through Effective Documentation With ClickUp
The SOAP approach gives structure to note-taking in a very dynamic and vital industry. As a documentation approach, it helps deliver better treatment plans, ensures compliance, and serves as records for future reference.
With a solid grasp of the key practices and concepts involved, you can now create effective SOAP notes. Combined with ClickUp’s tools, your productivity levels will surely grow by leaps and bounds. Sign up on ClickUp today.